Interesting Cases in Private Neurosurgical Practice
Anything related to the Central Nervous System has traditionally been a scare for us during Medical Training. Neuroanatomy, Neurophysiology, Neurological cases etc were the worst parts of our graduation days. This phobia continued into post-graduation and only those who end up doing Neurology or Neurosurgery are able to overcome it. In the course of my Neurosurgical practice, I meet many doctors who find neurological cases a nightmare. Also there is still considerable pessimism associated with outcome of neurosurgical cases. So I thought I should share some cases which are unique either in their presentation or in their encouraging outcomes.
Syndrome of the Trephined
A senior general practitioner from Pune had a Severe Head Injury in March 2009. He was GCS 7/15 with left dilated pupil. CT Scan showed a large Left Fronto-Temporo-Parietal Subdural Hematoma with mass effect and midline shift. He underwent a large craniectomy and evacuation of Subdural Hematoma. The Bone flap was not replaced by the surgeon because of severe brain swelling. The patient had a remarkable recovery and was conscious and ambulant after 10 days. One month after the first surgery, he became progressively drowsy and a repeat CT scan showed hydrocephalus. He was drowsy but arousable and obeying simple commands and moving all limbs. The surgeon placed a Ventriculo-Peritoneal Shunt on the right side. After the shunt, the patient rapidly deteriorated and became vegetative.
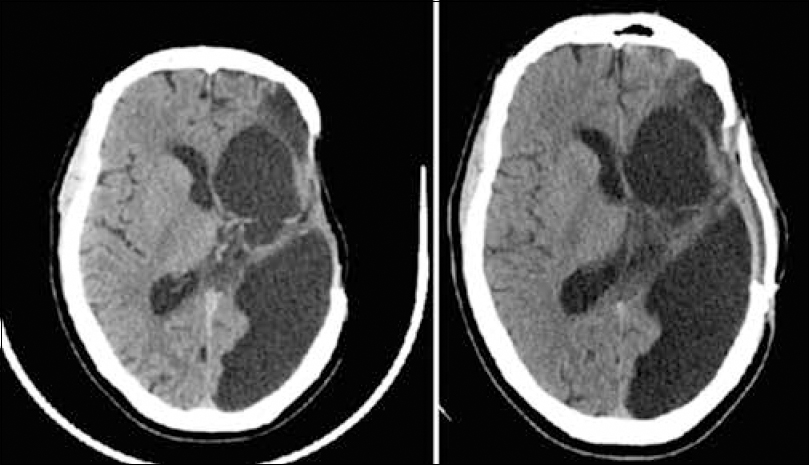
When I first saw him in July 2009, he had only spontaneous eye opening, not obeying with severe spastic right hemiparesis. The craniotomy defect was sunken deep and the shunt chamber was collapsed. A clinical diagnosis of Syndrome of the Trephined was made and CT Scan and MRI were asked for. The Scans showed severe shift of the brain structures to the right with severely chinked ventricles (Figure 1). After detailed discussion with the family which included few doctors from the Western Suburbs, it was decided to cover the craniotomy defect.
The patient was subjected to Autologous Cranioplasty using his own bone flap which was preserved in his abdominal wall. It was a pleasant surprise to all of us when he became completely conscious the same evening and his right hemiparesis disappeared (Figure 2). He walked out of the hospital after 3 days.
Syndrome of the trephined is when the atmospheric pressure directly acts on the brain in patients who have undergone surgical bone flap removal. The flap sinks producing an ugly cosmetic picture, but rarely it may produce clinical symptoms. In this case, the VP Shunt exacerbated the problem by severely reducing the intracranial pressure. The ventricles collapsed and the atmospheric pressure acted directly on the brain with resultant vegetative state and right hemiparesis.
Progressive contralateral hemiparesis, local pain and postural headache with cognitive and functional decline due to a skull defect have been reported and early cranioplasty has been recommended to prevent these phenomena.
Various factors like stretching of the dura and underlying cortex due to the atmospheric pressure, cicatrical changes occurring between the cortex, dura and the skin exerting pressure on the skull contents, and impairment of the venous return due to the atmospheric pressure acting on the region of skull defect with a resultant increase in the local external pressure have been implicated in the pathophysiology of the “syndrome of the trephined”.
The therapeutic value of cranioplasty has been proved by various experiments. Increase in cerebrospinal fluid (CSF) and superior sagittal sinus pressure, cerebral expansion, increase in CSF motion after cranioplasty due to an increase in cerebral arterial pulsations and improvement in cerebral blood flow, cerebral metabolism and cerebral vascular reserve capacity have been demonstrated after cranioplasty.
Unusual Presentation of Head Injury
A 21 year old labourer presented to the Hospital with history of heavy object on the head and upper back. He was conscious and obeying all commands. Cranial nerves and Upper limbs were normal, but he had complete paraplegia. Tone was normal. It was difficult to get a reliable sensory level due to language problems. Reflexes were depressed and plantars were upgoing. He was catheterised. In view of normal mentation and upper limbs, paraplegia was attributed to spinal injury and MRI of the spine was ordered. The MRI of the spine was completely normal. A rethinking of the case was done and a possibility of brain injury was suggested. MRI of the brain was done which revealed bilateral paracentral lobule hemorrhagic contusions (Figure 3). The patient was put on Anti-convulsants and Anti-edema measures and the paraplegia improved rapidly over 4-5 days. On discharge, there was no weakness of the lower limbs.
Head injury producing paraparesis has been described in few case reports. Anatomically the motor fibres to the lower limb lie in the medial most portion of the motor cortex and the paracentral lobule (Figure 4). The contusions in both leg areas produced the paraplegia in our case. Clinically, the absence of a sensory level and normal micturition would have helped us rule out a spinal injury, but sensory examination was unreliable and patient was catheterised on admission. Previous case reports have talked about bilateral vertex extradural hematomas and subdural hematomas producing paraparesis. Most of the cases recovered completely and rapidly like our case, once the pathology is treated.
The interesting message in this case is the importance of clinical examination to decide appropriate radiological investigations.
Time is Brain
A 76 year old lady presented to her General Practitioner with sudden history of left sided weakness since 45 minutes. She was a known case of hypertension and dyslipidemia. The doctor suspected stroke and immediately referred her to a to a tertiary stroke centre. He informed the stroke team and facilitated the admission procedure in order to save time. By the time we saw her, MR Angiography of the Brain and all blood investigations were done. She was conscious, with grade 2/5 power in the left upper limb and grade 3/5 power in the lower limb. She had left upper motor neuron type of facial palsy. MRA showed area of infarction in the right MCA territory and a large area of ischemia (penumbra). The right MCA was filling poorly (Figure 5). Since it was only 2 hours since symptom onset, we were within window period for Intra-venous thrombolysis. All contraindications for thrombolysis were ruled out and the family consent was taken. rTPA was administered according to the protocol and she was monitored in the Stroke Unit ICU.
The patient did well and power improved in 24 hours. Repeat MRA showed a small area of infarction in the right MCA territory. The ischemic zone was perfused well. The poorly filling Right MCA was now filling well up to the distal cortical branches (Figure 6). At the end of 5 days, she was walking with minimal support of a walker. Upper limb power improved to nearly 4/5.
I.V. rTPA treatment, 0,9 mg/kg, maximum of 90 mg), with 10 % of the dose given as a bolus , followed by an infusion lasting 60 min, is recommended within 3 hours after the onset of ischemic stroke. Intra-arterial treatment of acute MCA occlusion in a 6 hour-time window using pro-urokinase results in a significantly improved outcome. Mechanical thrombolysis using Penumbra Device improves outcome in a 8-9 hour time window. Time windows in posterior circulation stroke can be extended to 12-24 hours.
Brain attack or STROKE should be considered an Acute emergency like Heart Attack and referred immediately to a Tertiary Stroke Unit. The doctor who sees the patient first has to set the ball rolling by informing the casualty, radiologist and stroke specialist so that the time window is not lost. With protocol based Stroke Units, the outcomes of stroke have improved and with more awareness, we expect more patients to reach in time and get the benefit of Thrombolysis.
The quality of life after a stroke takes a toll on the patient, his family and the society. The time windows make it necessary for all doctors to recognize and refer stroke patients to stroke specialists and units IMMEDIATELY.
Is Age a Criterion to offer/refuse Neurosurgery
A 94 year old lady with no pre-morbid diseases had a trivial fall at home. Few days after the fall, she became progressively drowsy and was admitted to a Hospital. All routine investigations were within normal limits. MRI Brain was done which showed bilateral large Fronto-Temporo-Parietal Acute on Chronic Subdural Hematomas. When I saw her, she had spontaneous eye opening, but was not obeying commands. She had spastic quadriparesis and was unable to speak. Surgical drainage of the Subdural Hematoma was the only available option and it was offered to the family. The main concern was safety and outcome in view of advanced age. With some persuasion and encouragement, the extended family agreed for surgery.
The hematomas were drained under Local Anesthesia with Sedation. The lady recovered well and by Day 2 was alert and moving all four limbs. At the time of discharge on Day 4, she was eating orally, walking with minimal support, chatting and joking with her great-grandchildren!
There is no diagnostic or therapeutic enigma in this case but it highlights the issue of age. We always like to see the biological age of the patient rather than chronological age before offering surgery. Our patient was a sprightly, independent lady with no age related diseases and she deserved a chance to be self-sufficient again. Age alone cannot be a criterion to withhold treatment or surgery and it is important that we explain this to the family with measured optimism.
With increasing life expectancy in India, we will be faced with such circumstances often and we must consider pre-morbid condition and respect quality of life of the patient.
Delayed Diagnosis of Brain Tumor
A 42 year old Lady was admitted with seizures and altered sensorium. She was investigated for all metabolic causes and a CT Brain was also done. All blood investigations were normal. On examination, she was conscious, obeying simple commands. There was no limb weakness. Ophthalmological examination showed bilateral optic atrophy and severely diminished visual acuity. CT scan of the brain showed a large anterior cranial fossa tumour. MRI showed that the tumour was engulfing the optic apparatus and anterior cerebral artery complex and producing cerebral edema (Figure 9). On further history taking, it was found that she had been suffering from headaches since few years. She also had some behavioural changes for which she was under psychiatric care. The patient was on anti-psychotic treatment since 3 years. There was no scanning of the brain done before the current admission and now the tumour had grown to an alarming size with severe visual deficit.
Anterior cranial fossa tumors present with psychiatric symtoms like apathy, memory loss, psychotic behaviour etc. In contrast with the “negative ” symptoms of apathy, unconcern, and dementia which characterize lesions of the dorsal and middle portions of the frontal lobes, lesions affecting the base of the frontal lobes or orbital cortex and extending back to the infundibular region may be marked by ” positive ” symptoms-that is, excitement, disinhibition and euphoria.The patient may also present with hormonal changes or visual symtoms. A detailed history, examination and ophthalmological testing are mandatory. Perhaps we should have a low threshold for radiological investigations and at least CT Brain should be done before labelling a patient functional.
This patient probably lost valuable time before diagnosis which made her surgery difficult and outcome guarded. Time and again, we encounter such cases where diagnosis of pituitary adenoma, brain tumours, dural fistulae have been missed making their management difficult.
In the interest of the patient and so that we ourselves don’t get involved in litigation issues, it may be better to be liberal with radiological screening.
Dr. Viswanathan Iyer is a Consultant Brain and Spine surgeon. His special interest is Neurovascular Diseases, Stroke and Neuro-intervention.